 Yesterday while visiting my daughter in Palo Alto I was amazed at the long lines out the door and around the corner in two directions waiting to purchase the new iPhone X. Theses phones are selling for over $1,000.00 a piece. A phone for over $1,000, does this make sense? In this small city/town, I saw so many high-end cars. I’m now having concerns regarding our values and ethics. What is happening to our society? We seem to solve our problems and attempt to make us feel good by throwing money at whatever our problems instead of becoming self-reliant and accountable. More on this later.
Yesterday while visiting my daughter in Palo Alto I was amazed at the long lines out the door and around the corner in two directions waiting to purchase the new iPhone X. Theses phones are selling for over $1,000.00 a piece. A phone for over $1,000, does this make sense? In this small city/town, I saw so many high-end cars. I’m now having concerns regarding our values and ethics. What is happening to our society? We seem to solve our problems and attempt to make us feel good by throwing money at whatever our problems instead of becoming self-reliant and accountable. More on this later.
2015 was the worst year for drug overdose deaths. And then 2016 came along. If nothing is done, we can expect a lot of people to die: A forecast by STAT concluded that as many as 650,000 people will die over the next 10 years from opioid overdoses — more than the entire city of Baltimore. The US risks losing the equivalent of a whole American city in just one decade.
That would be on top of all the death that America has already seen in the course of the ongoing opioid epidemic. In 2016, more than 64,000 people died of drug overdoses in America — with synthetic opioids (such as fentanyl), heroin, and common opioid painkillers (like Percocet and OxyContin) topping other causes of overdose, according to new data from the Centers for Disease Control and Prevention. That’s a higher death toll than guns, car crashes, and HIV/AIDS ever killed in one year in the US, and a higher death toll than all US military casualties in the Vietnam and Iraq wars combined.
If you want to understand how we got here, there’s one simple explanation: It’s much easier in America to get high than it is to get help. In talking about this, Brandeis University opioid policy expert Andrew Kolodny draws a comparison to New York City’s fight against tobacco. In his telling, the city took a two-prong approach: It made tobacco less accessible — by banning smoking in public spaces and raising taxes to make cigarettes much more expensive. But it also made alternatives to tobacco more accessible — by opening a phone line that people can use to get in touch with a clinic or obtain free nicotine patches or free nicotine gum. It has seen its smoking rate steadily drop, from 21.5 percent in 2002 to 14.3 percent in 2015.
Essentially the opposite has happened with opioids. Over the past couple of decades, the health care system, bolstered by pharmaceutical companies, flooded the US with opioid painkillers. Then illicit drug traffickers followed suit, inundating the country with heroin and other illegally produced opioids, particularly fentanyl, that people could use once they ran out of painkillers or wanted something stronger. All of this made it very easy to obtain and misuse drugs.
Meanwhile, there has been little attention to getting people into treatment. According to the surgeon general’s 2016 report on addiction, only 10 percent of people suffering from a drug use disorder get specialty treatment. The report attributed the low rate to shortages in the supply of care, with some areas of the country lacking affordable options for treatment — which can lead to waiting periods of weeks or even months just to get help.
When you put these two issues together, you get the recipe for a disaster — one that has been only further accentuated by the socioeconomic and mental health issues that have plagued the US for years.
This is the story of the opioid epidemic: a crisis that has already taken hundreds of thousands of lives and is likely to kill hundreds of thousands more over at least the next decade if nothing is done.
How America’s opioid epidemic began
The opioid epidemic began in the 1990s when doctors became increasingly aware of the burdens of pain. Pharmaceutical companies saw an opportunity and pushed doctors — with misleading marketing about the safety and efficacy of the drugs — to prescribe opioids to treat all sorts of pain. Doctors, many exhausted by dealing with difficult-to-treat pain patients, compiled — in some states, writing enough prescriptions to fill a bottle of pills for each resident.
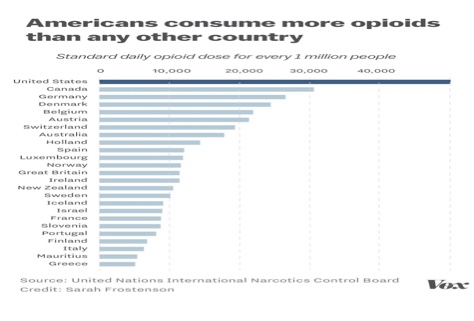
The drugs proliferated, making America the world’s leader in opioid prescriptions. As Stanford drug policy expert Keith Humphreys previously noted, “Consider the amount of standard daily doses of opioids consumed in Japan. And then double it. And then double it again. And then double it again. And then double it again. And then double it a fifth time. That would make Japan No. 2 in the world, behind the United States.”
The statistics really do back this up. Japan is one of the lowest prescribers of opioids in the developed world (for reasons outlined by Ella Nilsen for Vox). And the US absolutely dwarfs anyone else in terms of opioid prescriptions, with Japan not even showing up in the top 25:
Several key factors contributed to this.
First, there were the pharmaceutical companies. Wanting to make as much money as possible, these companies marketed their drugs as safe and effective for treating pain — even though the evidence for opioids shows that, particularly for chronic pain, the risks outweigh the benefits in most, but not all, cases. Many doctors and patients were convinced by this campaign. (Purdue Pharma, the maker of OxyContin, and some of its higher-ups later paid more than $600 million in fines for their misleading marketing claims, and opioid makers and distributors are now facing many more lawsuits on similar grounds.)
Then there were doctors. On one hand, doctors were under a lot of pressure from advocacy groups (some pharma-backed), medical associations, and government agencies to treat pain more seriously. On the other hand, doctors faced increasing pressure to see and treat patients quickly and efficiently.
The latter is a result of what Stanford addiction specialist Anna Lembke, author of Drug Dealer, MD, describes as “the Toyotazation of medicine — tremendous pressure on doctors within these large integrated health care centers to practice medicine in a certain way and get patients out in a timely fashion to be able to bill insurers at the highest possible level and to make sure that their patients were satisfied customers.”
Opioids provided an answer to these two problems. Doctors didn’t know how to deal with many of the complex pain problems their patients were dealing with because in many cases the answers were complicated and simply required too many resources and too much time. So an easy response was to give patients some pills.
In some situations, doctors simply prescribed far too much. With acute pain patients, doctors often gave weeks- or even months-long prescriptions when only a few days’ worth was needed. It was common, for example, to give weeks-long supply for opioids after wisdom teeth removals, even though the procedure usually leads to pain for no more than a week and the pain can typically be treated with milder painkillers like ibuprofen. The prescriptions left patients with a lot of extra pills, all because a doctor wanted to play it safe to avoid patient complaints.
And in other cases, the doctors involved were outright malicious — establishing “pill mills” in which they gave away opioids with little scrutiny, often for hard cash.
On the patient side, there were serious medical issues that needed to be addressed. For one, the Institute of Medicine has estimated that about 100 million US adults suffer from chronic pain. Given that the evidence shows opioids pose more risks than benefits in the majority of these cases, patients likely should obtain other treatments for chronic pain, such as non-opioid medications, special physical exercises, alternative medicine approaches (such as acupuncture and meditation), and techniques for how to self-manage and mitigate pain.
But these other options are often out of reach for pain patients. They may not have insurance to cover treatment. Even if they do have insurance, their health plan might not cover comprehensive pain care. And even if they do have insurance and their health plan covers pain treatments, there may not be a nearby pain clinic or doctor who can actually provide the care these patients are seeking. So frequently, the only suitable answer seemed to be opioids.
Opioids may still be a good answer for a few chronic pain patients. When prescribed carefully on a schedule that works to diminish the excessive buildup of tolerance, they can work for some people. But Stanford pain specialist Sean Mackey cautions that opioids should not be a first-line treatment due to the grave risks, and alternatives should be tried first.
With the broader proliferation of opioids, there were so many of these pills — enough prescribed just in 2015 to medicate every American around the clock for three weeks, according to the CDC — that they were often diverted: to teens rummaging through their parents’ medicine cabinets, other family members, friends of patients, and the black market.
As a result, the misuse of opioids and addiction to the drugs exploded. But painkillers were only the beginning. Heroin and fentanyl made the crisis much worse.
Over time, opioid users began moving to more potent kinds of opioids, particularly heroin and illicitly obtained fentanyl and its analogs. The reasons why varied; some did so after they lost access to painkillers, while others just wanted to seek out a stronger high.
Not all painkiller users went this way, and not all opioid users started with painkillers. But statistics suggest many did: A 2014 study in JAMA Psychiatry found 75 percent of heroin users in treatment started with painkillers, and a 2015 analysis by the CDC found people who are addicted to painkillers are 40 times more likely to be addicted to heroin.
As the crisis has gone on, an increasing amount of people with opioid addiction has even started on heroin. A 2017 study in Addictive Behaviors found that 51.9 percent of people entering treatment for opioid use disorder in 2015 started with prescription drugs, down from 84.7 percent in 2005. And 33.3 percent initiated with heroin in 2015, up from 8.7 percent in 2005.
That’s likely a result of increases in heroin and cutbacks in painkillers. As heroin proliferated across the US to match new demand from former painkiller users, excess in supply also gave more people new opportunities to try heroin even if they weren’t addicted to painkillers before. At the same time, painkillers have also become less accessible due to efforts to crack down on excessive prescriptions, limiting their availability as a gateway.
The result is that as opioid painkiller deaths leveled off over the past few years, heroin and particularly fentanyl deaths have rapidly increased. Synthetic opioids like fentanyl, in particular, are now linked to more drug overdose deaths than any other drug — even heroin and common opioid painkillers — in the US.
Heroin and fentanyl arguably pose even bigger risks than painkillers. Heroin is generally more potent, so it’s more addictive and more likely to cause an overdose. And fentanyl is even more potent than heroin, and it’s also often laced into illicitly sold heroin without a user’s knowledge — increasing the odds he’ll take a much bigger dose than he can handle.
As part of this shift, the crisis has also begun to afflict different people. Although prescription opioid overdose deaths have really hit middle-aged and older Americans in their 40s and up, there’s evidence that heroin and fentanyl are much more likely to hit younger adults in their 20s and early 30s — creating a divide in the epidemic by age.
The shift has also disproportionately hit the US’s Northeast and Midwest, where the rise of heroin and fentanyl have led to rapid increases in overdose deaths in states like West Virginia, New Hampshire, Ohio, and Pennsylvania.
As alarming as it may be, even the death toll arguably understates the depth of the crisis — because opioid misuse and addiction can lead to many more problems than death, from hindering social functioning to posing a huge financial strain since the drugs can be so costly. About 2.1 million people are estimated to have an opioid use disorder in America — and experts widely agree this is, if anything, an underestimate.
Other drugs can also be involved. A 2003 study found roughly half of heroin-related deaths involved alcohol, and the CDC found that 31 percent of prescription painkiller–linked overdose deaths in 2011 were also linked to benzodiazepines, a legal anti-anxiety drug.
In other words, this isn’t just an opioid painkiller crisis; it’s a full-on addiction epidemic, involving all sorts of legal and illegal drugs.
There are many reasons why addiction took off so easily, from poor access to mental health treatment to jobs leaving parts of the country to a growing sense of social isolation. Leo Beletsky, a professor of law and health sciences at Northeastern University, points to the fact that the US has seen rises in other deaths of despair, such as suicide and alcohol-related deaths, as proof that something deeper has gone wrong in American life.
“We have a lot of complex problems in this country,” Beletsky said. “Without really addressing all of those physical, emotional, and mental health problems, just focusing on the opioid supply makes no sense — because people still have those problems.”
The epidemic began with painkillers. Really? See the end of this post with the real numbers. But, as such, government agencies, regulators, doctors, and medical groups have pulled back on prescriptions for the drugs. Some states have limited how many opioids doctors can prescribe. The federal government put some opioids on a stricter regulatory schedule. Law enforcement has threatened doctors with incarceration and the loss of their medical licenses if they prescribe opioids unscrupulously. And the CDC released guidelines that, among other proposals, ask doctors to avoid prescribing opioids for chronic pain except in some circumstances. Hey, the last time I prescribed a narcotic for postoperative pain was 5 years ago.
This has had a steady effect on painkiller prescriptions, with total opioid prescriptions falling since 2010. But there’s still a lot of work to be done: In 2016, there were enough pills prescribed to fill a bottle for every adult in the US. And in 2015, the amount of opioids prescribed per person was more than triple what it was in 1999, according to the CDC.
There are risks to the pullback: With the existing population of opioid users, cutting them off from painkillers could be dangerous. Although they shouldn’t be a first-line treatment, opioids can be the only source of relief for a few chronic pain patients. If someone is suddenly yanked from a high dose of opioids, she could undergo painful withdrawal. (This is why experts say careful tapering is necessary for a patient getting off opioids — to ensure the process is as painless as possible.) And people who lose access to painkillers could decide that rather than deal with pain from withdrawal or chronic conditions, they’re going to get other opioids — such as heroin and fentanyl, which are deadlier than painkillers and would likely lead to even worse outcomes.
The shift to heroin and fentanyl is one reason experts emphasize the need for access to addiction treatment on top of efforts to pull back on painkillers.
“Let’s say you only focus on curtailing overprescribing to prevent people getting addicted, but you do nothing to expand treatment,” Kolodny said. “Then heroin and fentanyl will keep flooding in, and overdose deaths will remain at historically high levels until the generation that became addicted ultimately dies off.”
But based on the 2016 addiction report by the surgeon general, comprehensive treatment still remains out of reach for many. While the federal government has added some spending to addiction care (including $1 billion over two years in the 21st Century Cures Act), it’s nowhere near the tens of billions every year that Kolodny and other experts argue is necessary to fully confront the crisis. For reference, a 2016 study estimated the total economic burden of prescription opioid overdose, misuse, and addiction at $78.5 billion in 2013, about a third of which was due to higher health care and drug treatment costs. So even an investment of tens of billions could save money in the long run by preventing even more in costs.
For opioids, much of that funding needs to go to medication-assisted treatment (MAT), when medicines like methadone, buprenorphine, and naltrexone are used to combat opioid cravings. Several studies have found that MAT can cut mortality among opioid addiction patients by half or more. The CDC, the National Institute on Drug Abuse, and the World Health Organization all acknowledge its medical value. And experts often describe it as “the gold standard” for opioid addiction treatment — although, they caution, the medications won’t work for everyone, and other treatments should also be available.
But MAT remains inaccessible, in large part due to strict policies surrounding it. For example, the federal government still caps how many patients doctors can prescribe buprenorphine to, with strict rules about raising the cap. A HuffPost analysis found that even if every doctor who could prescribe buprenorphine did so at the maximum rate in 2012, more than half of Americans with opioid use disorders could not get the medication.
Even if all of this is fixed, however, the reality is some people will still misuse and get addicted to drugs. That’s one reason experts have also called for harm reduction efforts: Prescription heroin, which has been tried successfully in Canada and Europe, could let people access a clean supply of the drug. Supervised injection facilities could provide a space for drug users to inject illicit substances, with medical staff ready in case something goes wrong. Needle exchange programs could let people trade in used syringes for new ones, reducing the risk that a needle will carry HIV, hepatitis C, or some other disease. The opioid overdose antidote naloxone could be made more accessible across the country.
One concern with harm reduction strategies, echoed by anti-drug groups like the Drug-Free America Foundation, is that removing some of the risks to using harder drugs will perhaps make some people more likely to use dangerous substances.
But this simply has no foundation in the evidence. For example, a 1998 study by researchers at Johns Hopkins University found needle exchange programs generally reduced the spread of HIV without increasing drug use. A 2004 study from the World Health Organization, which analyzed two decades of evidence, produced similar results.
Harm reduction efforts will not prevent all deaths. They won’t make all heroin use safe. But they will reduce the amount of harm done by these drugs.
The policy solutions have to address all of these issues
As I explained in a last week’s post about how to stop the opioid epidemic, real policy solutions will have to address all of these gaps in America’s response to addiction. Experts say that prevention, treatment, and harm reduction all have a role to play.
Some experts argue the policy response will have to go even further — to also address the lack of access to adequate pain care and the root causes of addiction, particularly the socioeconomic and mental health problems that are commonly linked to drug use.
When experts were asked for specific proposals to deal with the root causes of drug addiction, each person seemed to have dozens of ideas: developing stronger social safety net policies, creating new job programs, offering better wraparound social services, better integrating mental health care with the rest of the health care system, encouraging non-drug sources of relaxation and entertainment, and on and on.
“It will really require rebuilding communities from the ground up,” Lembke said. “We have to help communities rebuild families. We have to give people meaningful work. We have to give people some opportunity for play — and by that, I mean alternative sources of dopamine, so people have something else to replace the drugs or prevent them from turning to drugs in the first place.”
In short, there’s no one silver bullet. America will have to do a lot at once.
There’s really wide agreement on this, yet so far governments haven’t done much. As I stated last week, Trump’s public health emergency declaration isn’t enough, only leveraging existing federal funds and waiving some regulations. While some states have boosted treatment and prevention, others, like Louisiana, Indiana, and Florida, have focused on ineffective “tough on crime” policies. And the public doesn’t seem to be putting much pressure on lawmakers to do anything about the crisis. As New York Times columnist Nicholas Kristof noted in a recent op-ed, opioids are “a mass killer we’re meeting with a shrug.”
Experts attribute this apathy to stigma: While doctors and experts know addiction is a medical condition, much of the public views it more as a moral failure.
Some rightly believe in “Darwin’s Theory, which says ‘survival of the fittest.’ Let these lost souls pay the price of their criminal choices and criminal actions. Society does not owe them multiple medical resuscitations from their own bad judgment, criminal activity, and self-inflicted wounds.”
Some lawmakers share this sentiment. Missouri State Sen. Rob Schaaf, a Republican, once remarked that when people die of overdoses that “just removes them from the gene pool.”
Perhaps the solution here is to educate people on the basic realities of addiction and why it needs our attention. The public needs to understand, as Lembke put it, that “if you see somebody who continues to use despite their lives being totally destroyed — losing their jobs, losing loved ones, ending up in jail — nobody would choose that. Nobody anywhere would ever choose that life. So clearly it is beyond this individual’s control on some level.” Until Americans understand that, it’s likely the policy response will remain inadequate. And hundreds of thousands could needlessly die as a result.
Until Americans understand that, it’s likely the policy response will remain inadequate. And hundreds of thousands could needlessly die as a result.
Maya Salam expanded more on the epidemic and stated rightly that the opioid crisis is a crisis years in the making. The current opioid epidemic is the deadliest drug crisis in American history. Overdoses, fueled by opioids, are the leading cause of death for Americans under 50 years old. As I pointed out already killing roughly 64,000 people last year, more than guns or car accidents, and doing so at a pace faster than the H.I.V. epidemic did at its peak.
I pointed out last week President Trump declared the opioid crisis a “public health emergency” on last Thursday, though he did not release additional funding to address it. Had he declared it a “national emergency,” as he promised to do in August, it would have led to the quick allocation of federal funds.
Ty Wight for the New York Times reported that even babies are affected by the crisis, with a surge of newborns dependent on opioids. The youngest members of society have not been exempt from the crisis. Toddlers and young children are increasingly being found unconscious or dead after consuming an adult’s drugs, and a surge of opioid-dependent newborns has forced doctors to rethink treatment.
Our reporters have been deciphering and providing context to masses of data about the many and varied ways opioids are affecting Americans.
Yousur Al-Hlou, Josh Katz, and Drew Jordan outlined the facts that it’s the deadliest drug crisis in American history. It kills about 90 Americans every day.
The government’s account of drug deaths in 2016 was the first national data to break down the growth by drug and by state, which revealed that deaths involving synthetic opioids, mostly fentanyl, had risen 540 percent in just three years.
While Mr. Trump fulfilled his vow to add urgency to the rapidly escalating opioid problem, his declaration falls short of the national emergency declaration he had pledged. These are the 28 currently active national emergencies.
Drug companies and doctors have been accused of fueling the opioid crisis, but insurers may also be playing a role by making it easier to get opioids than the drugs that treat addiction to them. One study states that a patient had to begin taking a hydrocodone, an opioid, to treat her pain after her insurer changed what it covered.
Dr. Thomas A. Andrew of New Hampshire stated that his own state of New Hampshire had more deaths per capita from synthetic opioids than any other state. Dr. Andrew decided to stop practicing medicine and instead minister to the living about the dangers of drugs. “I’m not an alarmist by nature, but this is not overhyped,” he said.
The Upshot reported on prescription drug monitoring programs, a tool that could be more widely used to fight opioid abuse. These programs are already being instituted in many States.
Heroin users are filling the country’s jails, but recovering addicts are almost always cut off from their medication while incarcerated. Connecticut, though, is trying something new: a methadone treatment program to help inmates successfully re-enter society.
On Staten Island, prosecutors are leaping into largely uncharted legal terrain to fight the scourge: charging dealers in overdose deaths.
Let me be real clear and I will make this comment again later the Internet is proving to be a grim tool in the opioid drug trade. On Reddit, one of the world’s largest online communities, opioid forums have offered a place to buy drugs and find solace for people like Rachel Frazier, who posted on Reddit regularly and dipped into drug-related communities such as “opiates.” She died two weeks after seeking drugs in a forum.
Dealers are embracing the dark web to anonymously send powerful synthetic opioids such as fentanyl to nearly every region of the country. Despite dozens of arrests, new merchants — many of them based in Asia — quickly pop up to fill the void.
The final report by President Trump’s Opioid Commission on the opioid crisis did not call “for new dollars to address the worst drug crisis in US history,” according to the AP (11/1, Johnson), instead of calling for “sufficient funds” to meet its recommendations. The commission suggested allowing the Office of National Drug Control Policy to review federal spending on the problem, calling for investment “in only those programs that achieve quantifiable goals and metrics” and calling for the ONDCP to “establish a system of tracking and accountability.” The report also urged, in the AP’s words, “streamlining funding to states by using block grants.” Other recommendations include establishing drug courts in all 93 federal judicial districts, more emergency responders being allowed to administer overdose reversal drugs, additional training for doctors, “and penalties for insurers that dodge covering addiction treatment.”
Bernstein of The Washington Post reported the commission offered 56 recommendations in “a wide-ranging menu of improvements,” including for the Centers for Medicare and Medicaid Services to no longer include questions about pain in hospital performance satisfaction surveys, which physicians say pressures them “to treat pain aggressively.” However, the commission did not endorse using “marijuana for pain, despite some studies suggesting that access to marijuana may decrease opioid deaths,” or creating safe injection sites for opioid users, such as exist in Canada.
As expected treatment advocates had “mixed” reactions to the report, “with many expressing frustration that the commission had not called for a specific level of funding.” The report did, however, recommend streamlining “fragmented” federal funds for addiction prevention and treatment into block grants that would require each state to file only a single application.
One point that we all are missing and I have brought this up before, the availability of heroin as well as fentanyl and other synthetic opioids is out of control as well as the price of these drugs. These drugs can be purchased through online sights from other countries and are promoted through social media.
You can throw all sorts of money at treatment centers, clinics, etc. but unless you control the availability, young and old will avail themselves of these drugs to get higher and higher. And who is profiting from this crisis? Drug cartels, gangs, drug companies and yes also the drug rehabilitation and pain centers are all making millions. I wanted to stop here in this very long post but this A.M. on Face the Nation there was an interesting interview. I will continue that thread next week as I discuss whether Docs are the problem.
The common thread is accountability and greed especially self-accountability. It’s always easier to pick a reason to place the blame, the guilt rather than self. In this case with opioids, the self should be considered the government itself and big pharma, but hey, they are “like” the government, and are part of that fabric too, Stop the blame game and get the opioids off the street!!!